Critical knowledge for critical care
Staying current on the latest changes in critical care guidelines can help you make the right decisions at the right time.
For hospitalists, there are few moments of greater pressure than dealing with a critically ill patient.
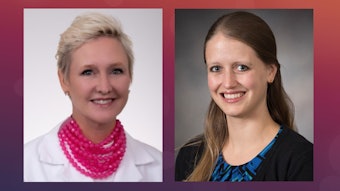
Jocelyn Zee, DO, FAAFP, SFHM, critical care physician with Acclaim Physician Group in Fort Worth, Texas, said that is one time that the hospitalist truly feels that all eyes are on them.
“Walking into a room with a critically ill patient or seeing someone take a turn for the worse can be quite harrowing—everyone in the room then turns to you for the answers,” she said. “In some situations, you are it, you are ‘the help.’”
Arming yourself with the latest information and advances in critical care can dramatically increase your opportunity for success and help you make the right choices in difficult cases.
Patricia Kritek, MD, EdM, professor of pulmonary care, critical care, and sleep medicine at the University of Washington in Seattle, said the Advanced Learning Course, “Turning Chaos Into Calm: Critical Care Management for Today’s Hospitalist,” will include sessions on ventilator management, shock, neurologic emergencies, toxidromes, and more. In addition, there will be two case-based sessions that will allow participants to walk through each case and make diagnostic and therapeutic decisions.
“One session will focus on patients with acute respiratory failure and the other is a collection of challenging cases,” Dr. Kritek said. “We’ve tried to highlight areas of debate and controversy in critical care like assessing volume responsiveness, what fluid to choose for resuscitation, and when to start a pressor. These are areas with conflicting results in trials and long-established practice patterns. I think many clinicians have strong opinions on what to do, and we don’t have definitive trial data that says ‘this is the one right way to do it.’”
Staying informed is crucial to making the right decisions in critical care. Updated Surviving Sepsis Campaign Guidelines were released by the Society of Critical Care Medicine in 2021. Dr. Zee said one of the more notable changes was a shift in the language from a “strong” recommendation for an initial fluid bolus of 30 mL/kg to a “weak” recommendation.
“The latest guidelines actually say ‘suggests’ instead of ‘recommends,’” Dr. Zee added. “They also recommend a balanced crystalloid solution over normal saline solution for resuscitation.”
Another change that stands out for Dr. Zee involves the administration of vasopressors.
“There might have been delays in the administration of vasopressors, since many believed they could only be initiated via central venous access, which can be limited depending on where you practice,” she said. “The 2021 guidelines speak to starting vasopressors immediately and peripherally and not having to wait until central access is established. Obviously, there are some caveats and careful monitoring that must occur with this.”
The course will also feature an update on airway management from Todd Rice, MD, associate professor of medicine at Vanderbilt University Medical Center in Nashville, and co-author of a study published in the Journal of the American Medical Association in 2021 that suggested the use of the bougie—a semirigid introducer that can be placed in the trachea to facilitate tracheal intubation—might improve intubation success on the first attempt.
“Our goal is to help hospitalists feel more comfortable with a wide array of critical illnesses as well as think through when it makes sense to call for help,” Dr. Kritek said.
Visit SHM Meeting News Central for more coverage.